聽過有許多人都有因網紅或廣告介紹買入保養品後不適合的慘痛經驗……所謂「別人的蜜糖,我的毒藥」,現在我用各種保養品最在意它的成分!是否太刺激?香味會不會太刺鼻?
我自己的保養步驟算簡單,臉部早晚清潔後簡單上化妝水→精華→乳液,僅有乳液區分夏天是清爽乳液、冬天是油脂成份較高的乳霜。身體也是區分冬夏,夏天用較水潤質地、冬天則著重保水保油。最後依近期肌膚狀況加入「重點產品」,例如最近因為家有新生兒,24小時待在冷氣房內很容易造成肌膚水分流失,臉頰出現小塊的局部乾燥;加上一堆嬰兒用品需要清洗消毒,大量接觸水及清潔劑的情況下,我很在意肌膚的保濕度及膚況穩定度。

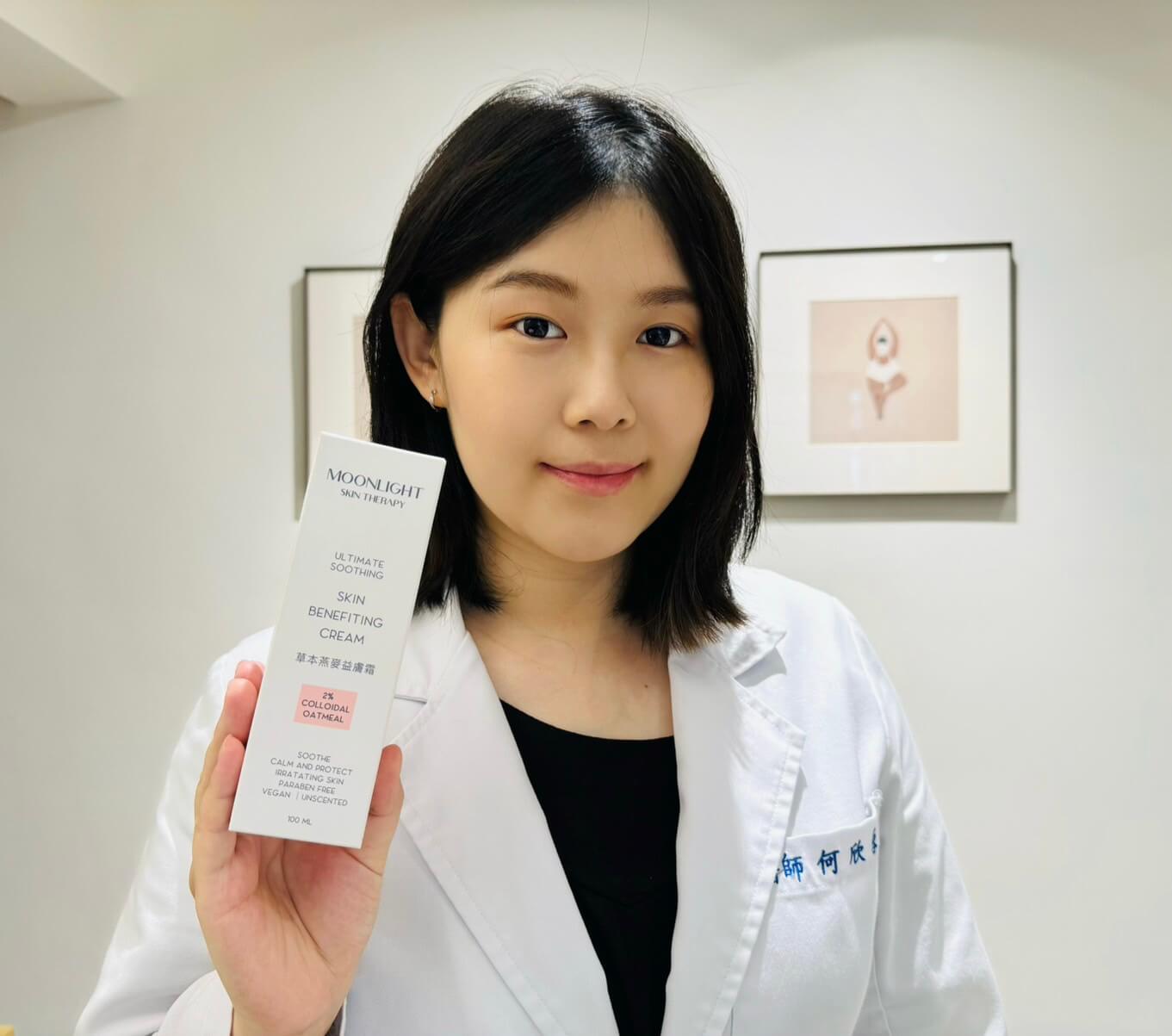
使用重點產品加強保濕時最害怕用完黏膩不透氣,撐不了多久就想洗掉,有些甚至還會造成皮膚癢,變成反效果。好險這次試用的Moonlight草本燕麥益膚霜吸收快速,不會厚重但也不會有擦了跟沒擦差不多的感覺。尤其我是個半夜容易在睡夢中抓手的人,除了定期用藥,最怕皮膚屏障被破壞。Moonlight草本燕麥益膚霜原本的開發理念就是小孩也可以用,例如如果用了凡士林等一般保水產品效果仍不彰。其內含「2%膠體燕麥+乳木果油+6種草本精草的SRS-6 repairing complex」,燕麥不僅是富含膳食纖維的寶藏食材,也能幫助維持膚況穩定。常用於護手霜的乳木果油,其滋潤效果能幫助皮膚表面形成保護膜,鎖住水分。

自從懷孕以後,對於各種香味太重的產品也開始避免,除了防止太過強烈的味道引起孕吐反胃,小孩出生後也會避免在身上留下強烈的氣味,希望讓小孩一直都能好好感受到「媽媽的味道」~Moonlight草本燕麥益膚霜無添加礦物油、石化成分、paraben防腐劑、香精,香精或香料一直是造成過敏常見原因,也是我目前選用保養品時特別注意避開的物質。
因此如果你跟我一樣也是敏弱肌,在尋找無過多添加物、可用於全身及臉的保濕產品,推薦試試Moonlight草本燕麥益膚霜,看它會不會也成為你的蜜糖~

【免責聲明】
瀏覽及使用本網頁內容者均視為同意及明確認知本協會為「非以營利為目的」之公益性社會團體,非營利事業單位,並無從事商品的生產、製造、銷售或廣告等行為,本網頁之設立及內容係以「專業醫學促進國家預防醫學發展」之討論與意見交流為目的,以上醫友心得分享為醫事相關人員實際體驗後所撰寫之真實個人意見,商品資訊之來源為商品廠商之公開資訊內容,不代表本協會及網站之立場,亦非本協會及網站之陳述,其真實性及合法性應由各商品廠商負最終且完全之法律責任。